Concern that omicron, the latest coronavirus variant, could be poised to overtake delta, which swept the globe in roughly two months since it was first identified, has steadily grown. But recent results suggest that current vaccines may target a region of the virus that’s relatively conserved among variants before omicron, allaying some fears that a new variant could totally dodge immune responses from first-generation vaccines.
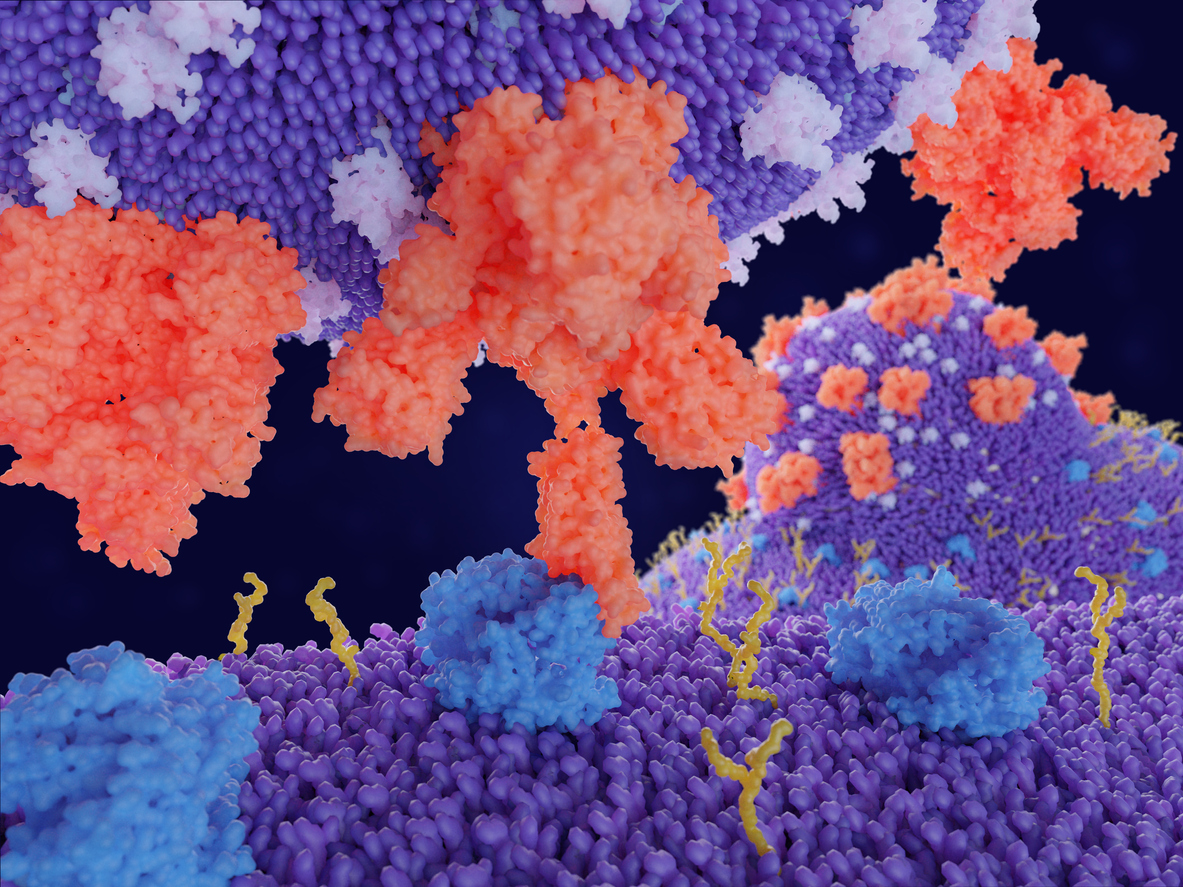
Variations of SARS-CoV-2, the virus that causes COVID-19, arise as the virus tweaks its genetic code. Each mutation is a bid to evade immune system defenses—teed up by vaccination or previous infection—and infect more people, more efficiently. Changes to the virus’ spike proteins, the molecular means by which the virus invades cells, are usually to blame for swift-spreading variants.
But in a recent study, researchers found that a key part of the virus’ spike proteins doesn’t change substantially. Scientists at the Institute for Protein Innovation joined a team of researchers led by Bing Chen, a virologist at Boston Children’s Hospital, to find that it would be difficult for new variants of the virus to completely evade immune responses that target that conserved region.
SARS-CoV-2 owes its infectivity to its spike proteins, which are tangles of amino acids that enable the virus to latch onto host cells and penetrate them. These spike proteins have two subunits, known as S1 and S2, that comprise a tip and stalk, respectively. Anchored in the virus’ outer wrapping, the S1 subunit locks onto receptors found on cells in the human respiratory tract, called ACE2 receptors, and pulls the rest of the virus in, relying on the S2 subunit to fuse virus and cell.
Researchers found that delta’s mutations caused minimal changes in the spike protein’s receptor binding domain, or RBD, which is on the S1 subunit. The results align with previous findings that the antibodies—or proteins that identify and neutralize invaders—produced by the immune systems of many people infected with SARS-CoV-2 were also pinpointing the RBD, signaling that the region is a key target for vaccine design and antibody treatment.
“That’s telling us that the RBD is so critical, the virus simply cannot mutate much away from the original structure,” Chen said.
The results indicate targeting the RBD could still be the best universal strategy for vaccine makers and could help calm fears around emerging variants.

Delta owes its dominance to efficient membrane fusion
Chen and his team actually began their study with a question that many had been asking: Why was the delta variant dominating the number of COVID-19 cases? Patients infected with delta have roughly 1,000 times more SARS-CoV-2 in their systems than those infected with previous variants and, though alpha was about 60% more transmissible than the initial strain of the virus, delta nonetheless took over.
“There must be something unique about this lineage, this variant,” he said. “We wanted to find out the molecular basis for its increased transmissibility and potentially the antibody resistance as well.”
Chen’s team made cells to produce spike proteins from prevalent strains of SARS-CoV-2: G614, alpha, beta, gamma, delta and kappa. Then, researchers mixed those cells with mammalian cells that produced ACE2 receptors, which expressed extra ACE2 receptors on their surfaces to ensure cells with spike proteins could detect them. But the scientists found that no variant fused any better than another
To the team’s surprise, however, delta was uniquely able to latch onto cells in Chen’s control group, which did not express additional ACE2 receptors. As the levels of ACE2 increased, the other variants could bind and eventually caught up to delta. The researchers concluded that delta gains its edge by fusing with human cells more effectively, even when their ACE2 receptors were scarce.
“That was sort of a surprise when we looked at the negative control—we thought it was negative control—but delta was actually sort of standing out,” Chen said.
In another experiment, scientists used another, less dangerous virus to express the spike protein and measured how rapidly the so-called pseudovirus infected cells. While other variants had relatively similar rates of membrane fusion, delta penetrated cells remarkably fast, particularly within the first hour.
“That really explains what’s being reported out there,” Chen said, “that the delta variant actually has much higher viral load compared to previous variants.”
In short, the mutations harbored by delta render the virus better able to fuse with cells with ACE2 receptors, rapidly infect them and release more virus along the way.
Now, a clear target for vaccines
In addition to quicker infectivity, Chen wanted to know if delta’s prowess was also due to an enhanced ability to evade immune system defenses. To find answers, he turned to IPI’s Wei Yang, Haisun Zhu and Krishna Anand. Using flow cytometry—which floats one cell at a time through a laser beam to reveal its physical and chemical properties—IPI researchers studied how well variants bound and adhered to neutralizing antibodies from COVID-19 patients.
“The main advantage for IPI is that we can do this in a high-throughput way,” Zhu said.
In the body, antibodies bind and hold onto a part of the SARS-CoV-2 spike protein, blocking it from otherwise docking to the ACE2 receptor and infecting cells. In Yang, Zhu and Anand’s experiments, antibodies from three patients targeted the RBD region, two bound to the NTD and one hooked onto the entire S2 subunit.
IPI researchers found that mutations in the delta variant’s NTD region allowed it to evade immune detection by antibodies targeting that region. Alternatively, antibodies that honed in on the RBD still bound to delta and neutralized the virus, which the subsequent pseudovirus assays confirmed.
The results extended to each strain of the virus, from alpha to kappa: Each used a different strategy to remodel its NTD and evade host immunity. By contrast, all variants have strictly preserved the overall structure of their RBD, affirming its critical role in ACE2 receptor binding.
To Chen, these findings bear out the best strategy to fight the pandemic: Design preventative vaccines and therapeutic antibodies that target the RBD region of SARS-CoV-2.
Will this strategy apply to omicron? It might, depending on the location and consequences of its cumulative mutations. Some scientists have already reported that a small number of RBD-targeting antibodies can indeed neutralize omicron despite the roughly 15 mutations to its RBD, Chen said. Antibodies targeting the NTD have failed.
Right now, Chen is working to improve scientists’ understanding of the virus overall by also studying the spike proteins of other coronaviruses to trace their evolution.
“We can figure out how the coronavirus evolved from the bat to pathogens with pandemic potential,” he said. “Ultimately, that can help us design a so-called ‘pan-coronavirus vaccine’ that will prevent this type of thing from happening again in the future.”
Funding for this study came from Emergent Ventures, the Massachusetts Consortium on Pathogen Readiness and the National Institutes of Health.
Writer: Halle Marchese, halle.marchese@proteininnovation.org
Sources: Bing Chen, media.relations@childrens.harvard.edu;
Haisun Zhu, haisun.zhu@proteininnovation.org